Promoting Safe Sleep while Protecting Neurodevelopment: The Dandle® WRAP Stretch
“Hospitalized preterm infants should be placed supine as soon as clinical status has stabilized and they have achieved positional stability, that is, when therapeutic or non-supine positioning is no longer medically indicated. This milestone is usually achieved by 32 weeks’ gestational age.”
(AAP, 2022).
Following the recommendation of the American Academy of Pediatrics (AAP) (Committee on Fetus and Newborn, 2022), many NICUs enact Safe Sleep parameters at around 32 weeks postmenstrual age, which often involves removing all developmental positioning supports in an effort to model Safe Sleep for parents.
Although implementing back to sleep as early as 32 weeks postmenstrual age is recommended, it is important to consider the musculoskeletal and sensory organizational processes occurring in the infant between 32 weeks and term gestation. These factors should be considered when determining “positional stability”:
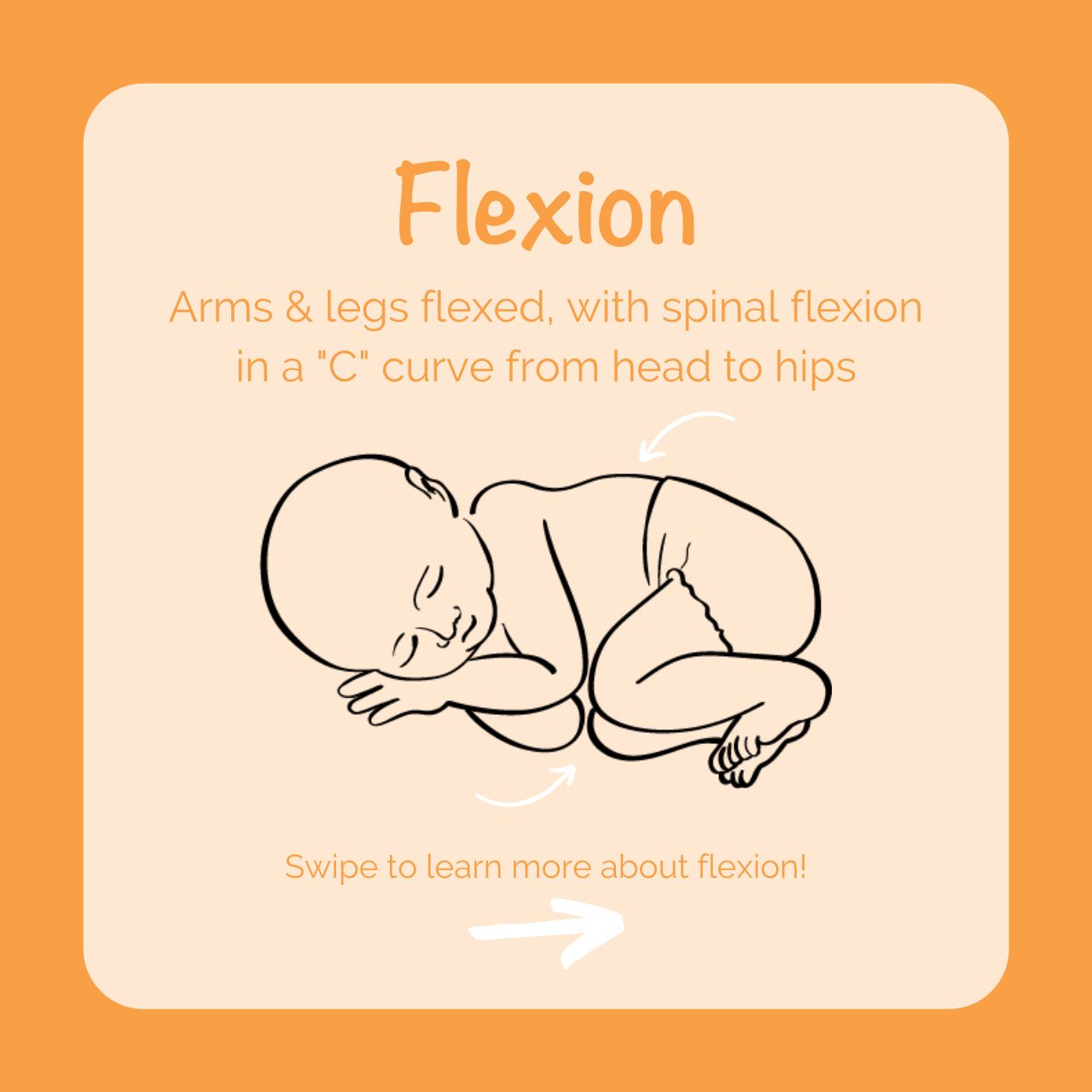
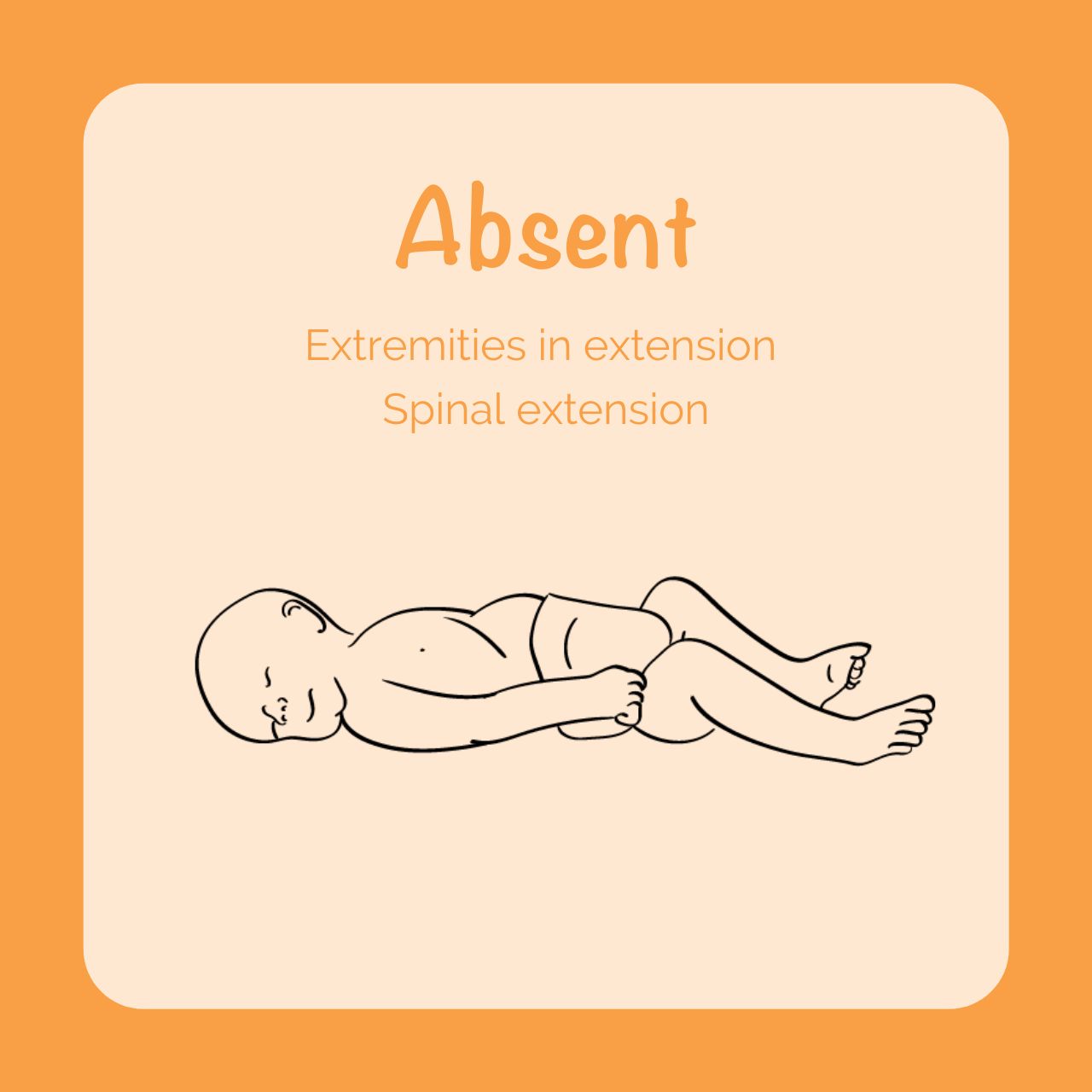
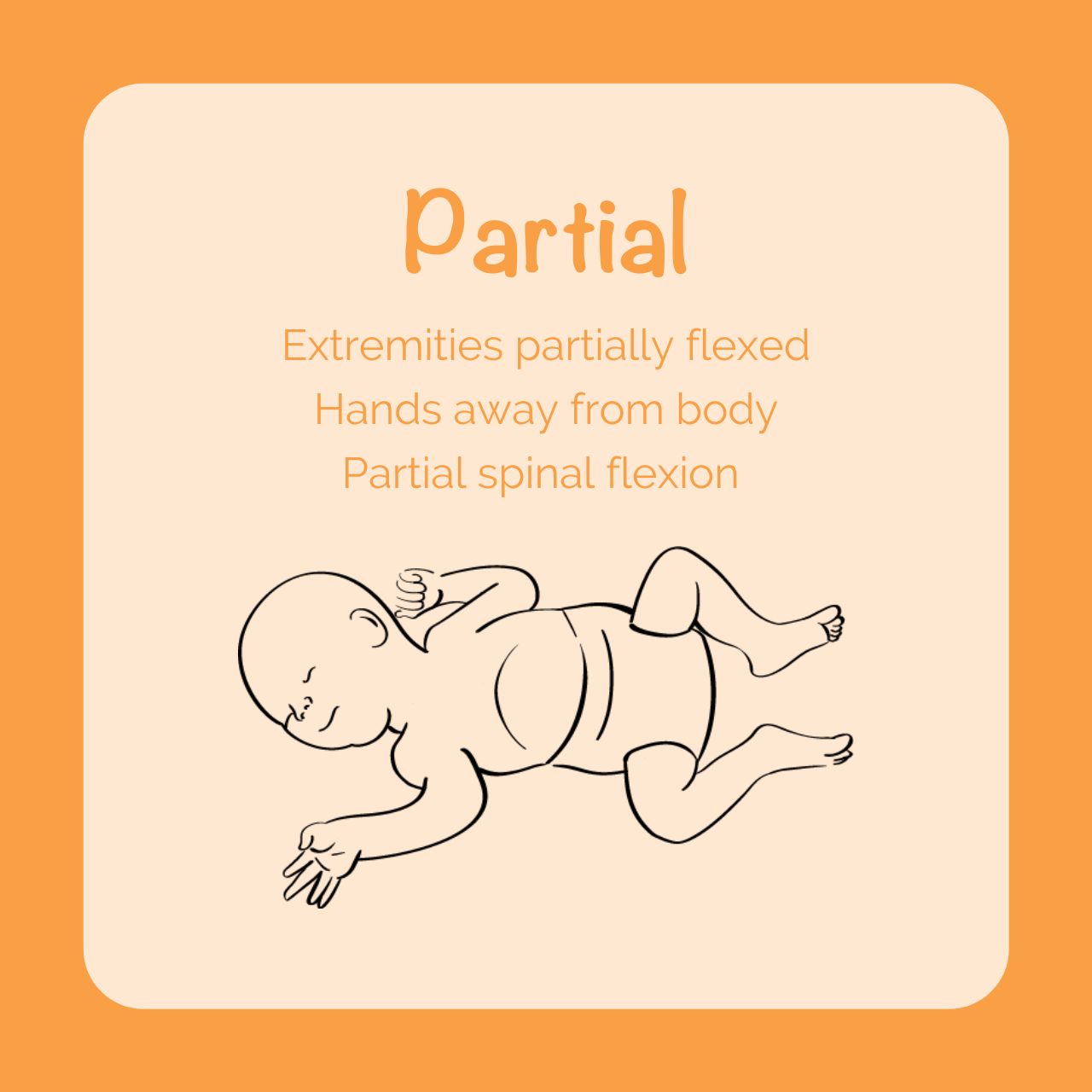
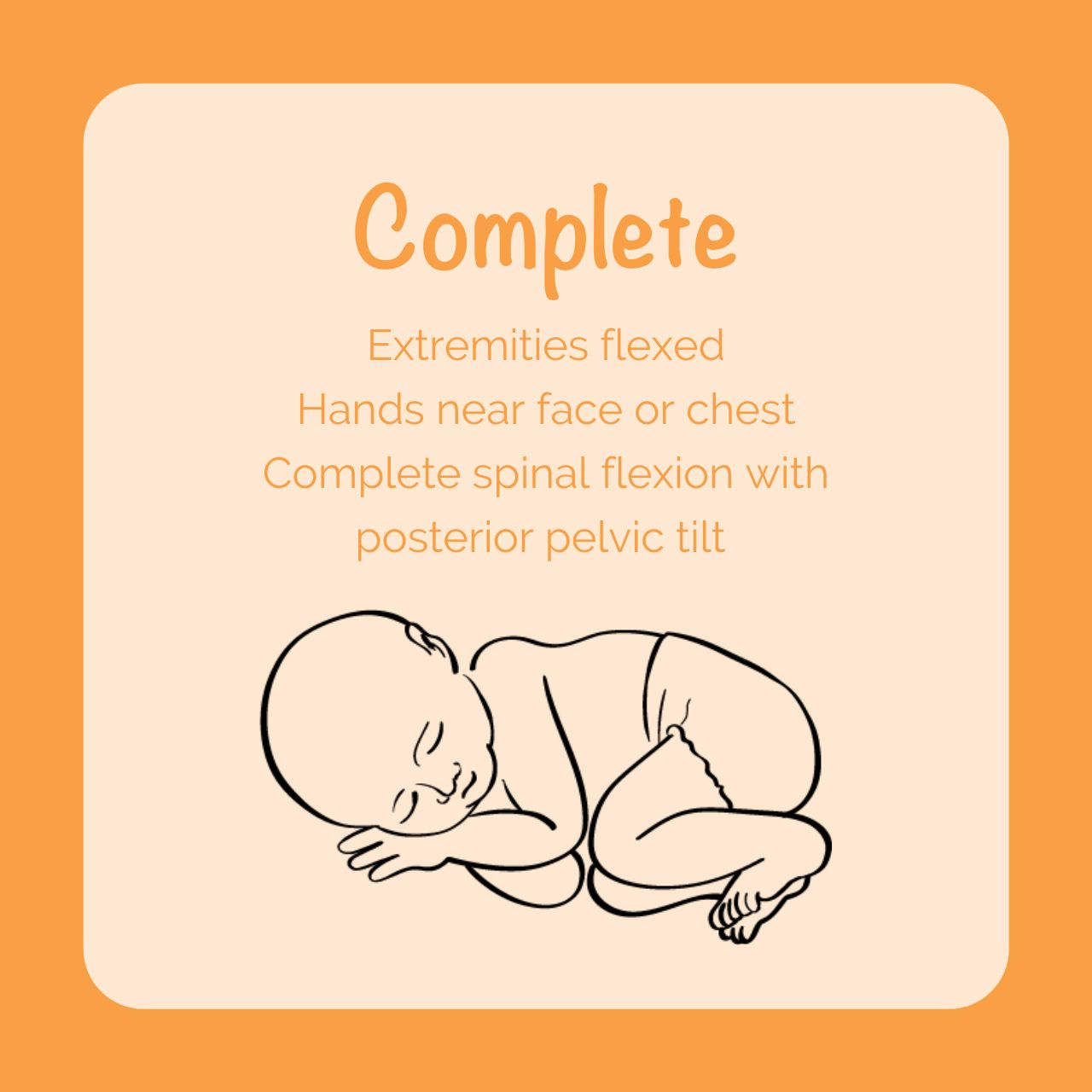
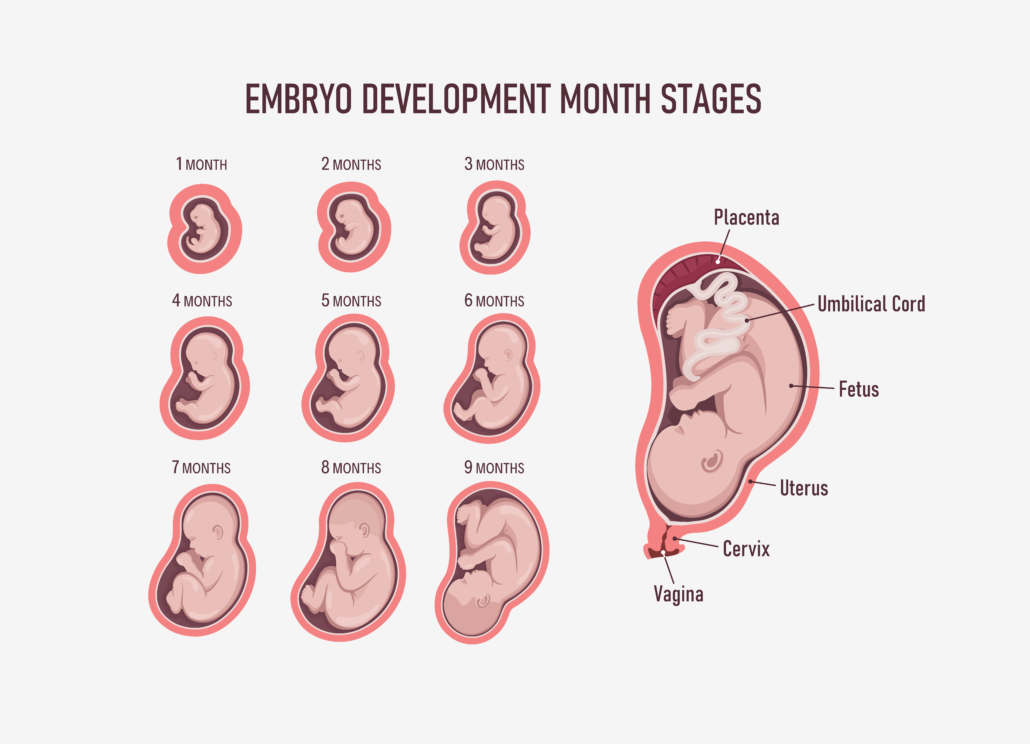
- Development of physiologic flexion posture as the foundation of normal motor development matures in the last weeks of pregnancy.
- Joint compression and resistance to active extension necessary for bone development is most prevalent in the last trimester of pregnancy.
- Calcium and phosphorus acquisition for bone ossification is maximized in the third trimester of pregnancy.
- The degree of prematurity directly affects an infant’s ability to maintain positional stability secondary to medical equipment required to support respiration and digestion, immaturity or atypical development of the central nervous system requiring cardiopulmonary monitoring, and possibly delayed skeletal maturation.
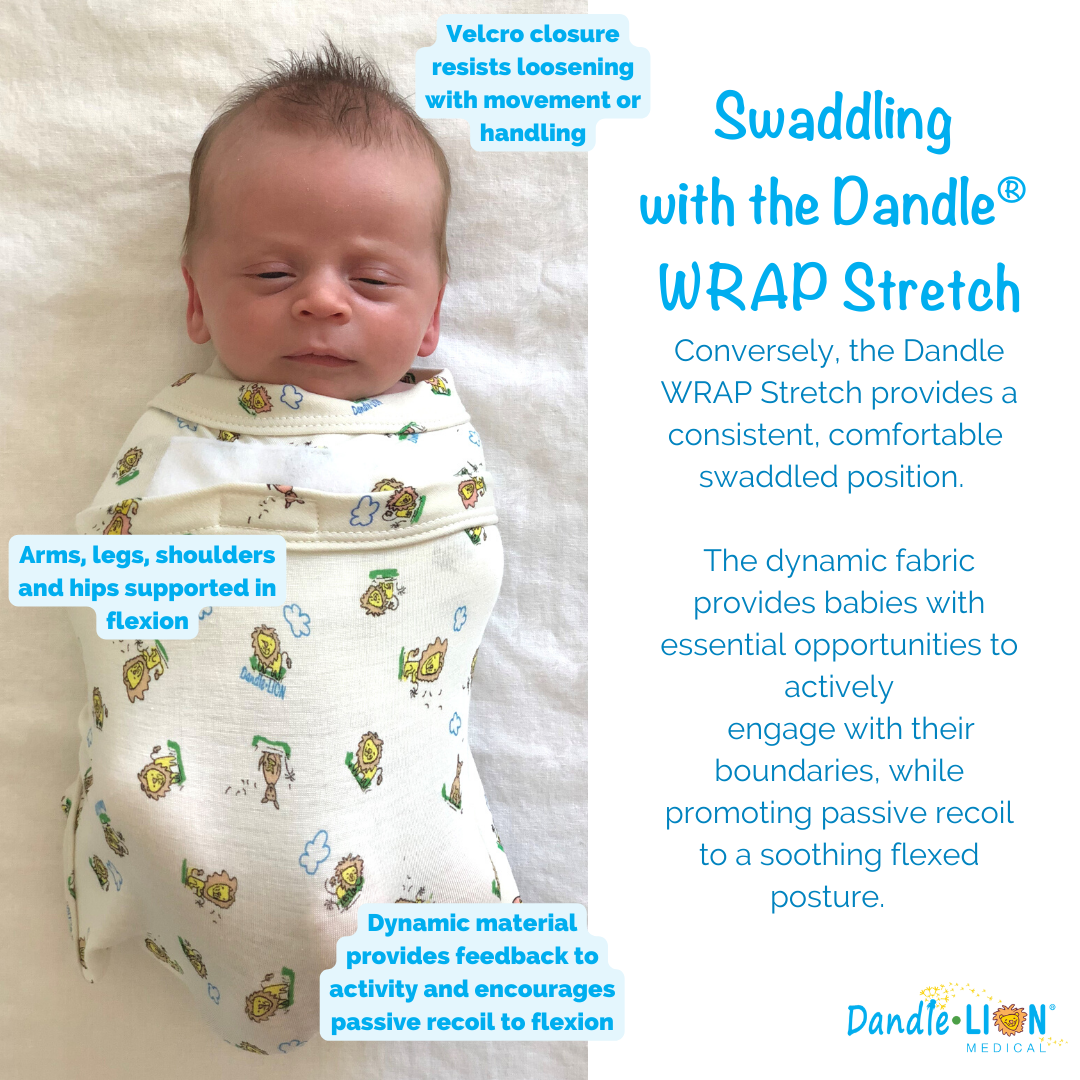
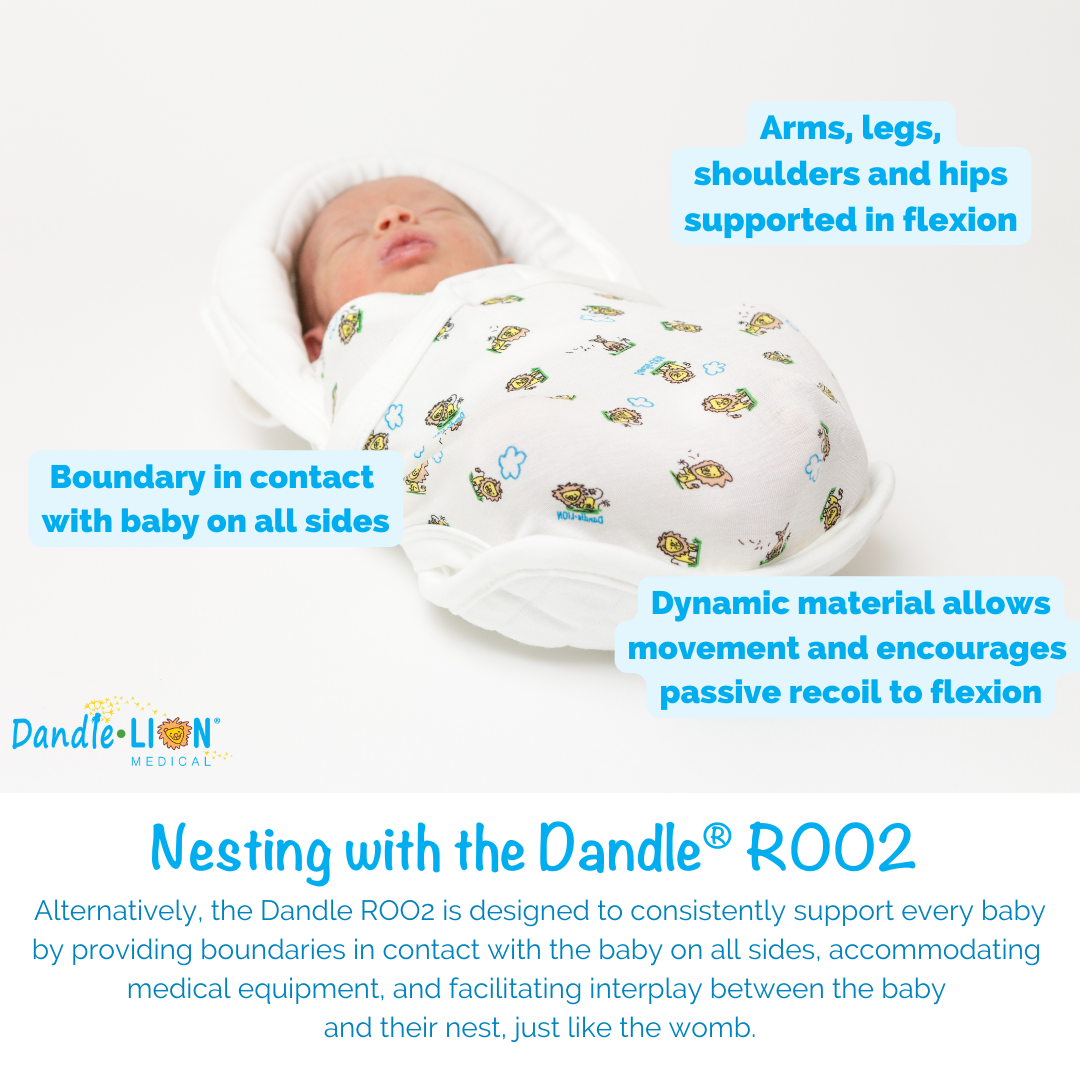
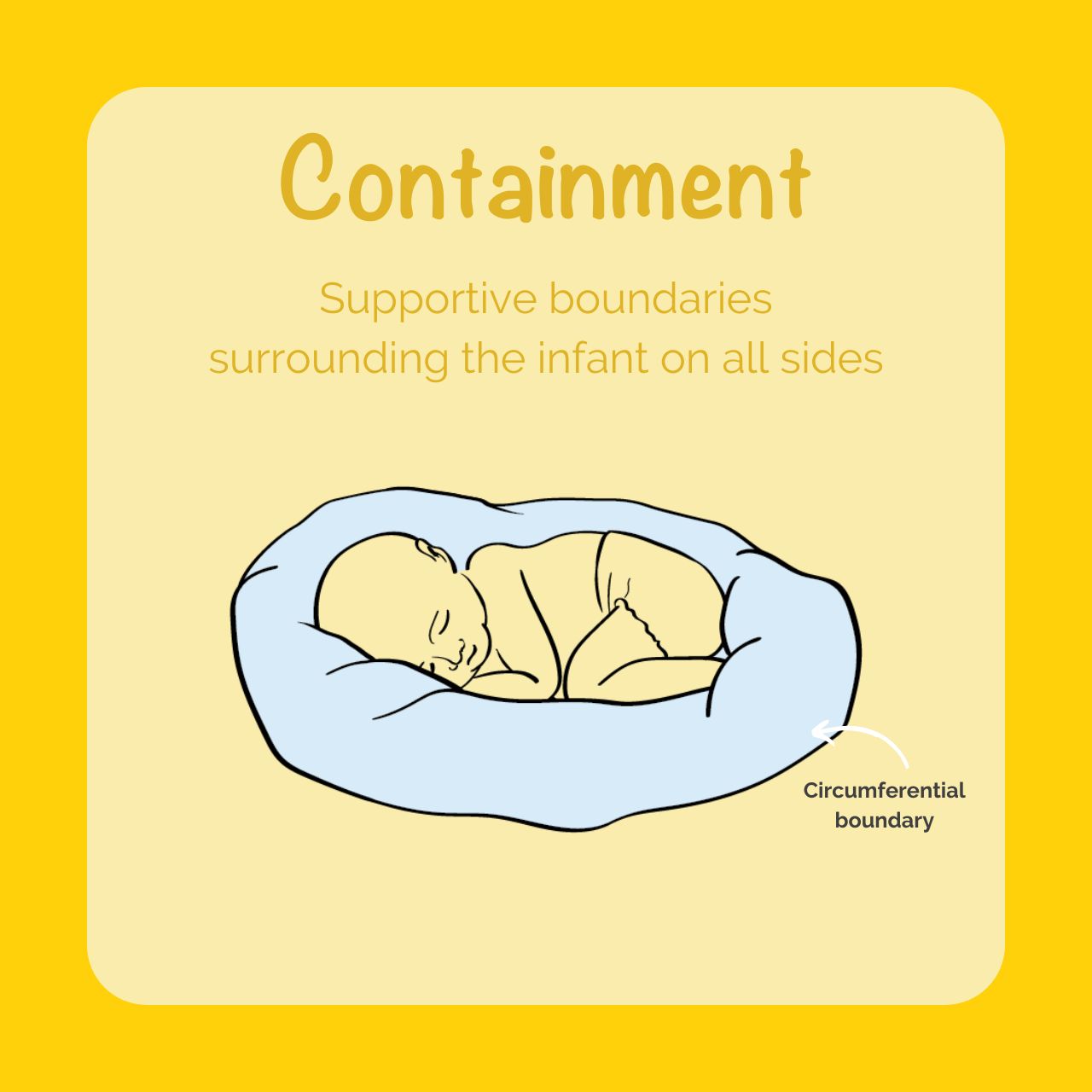
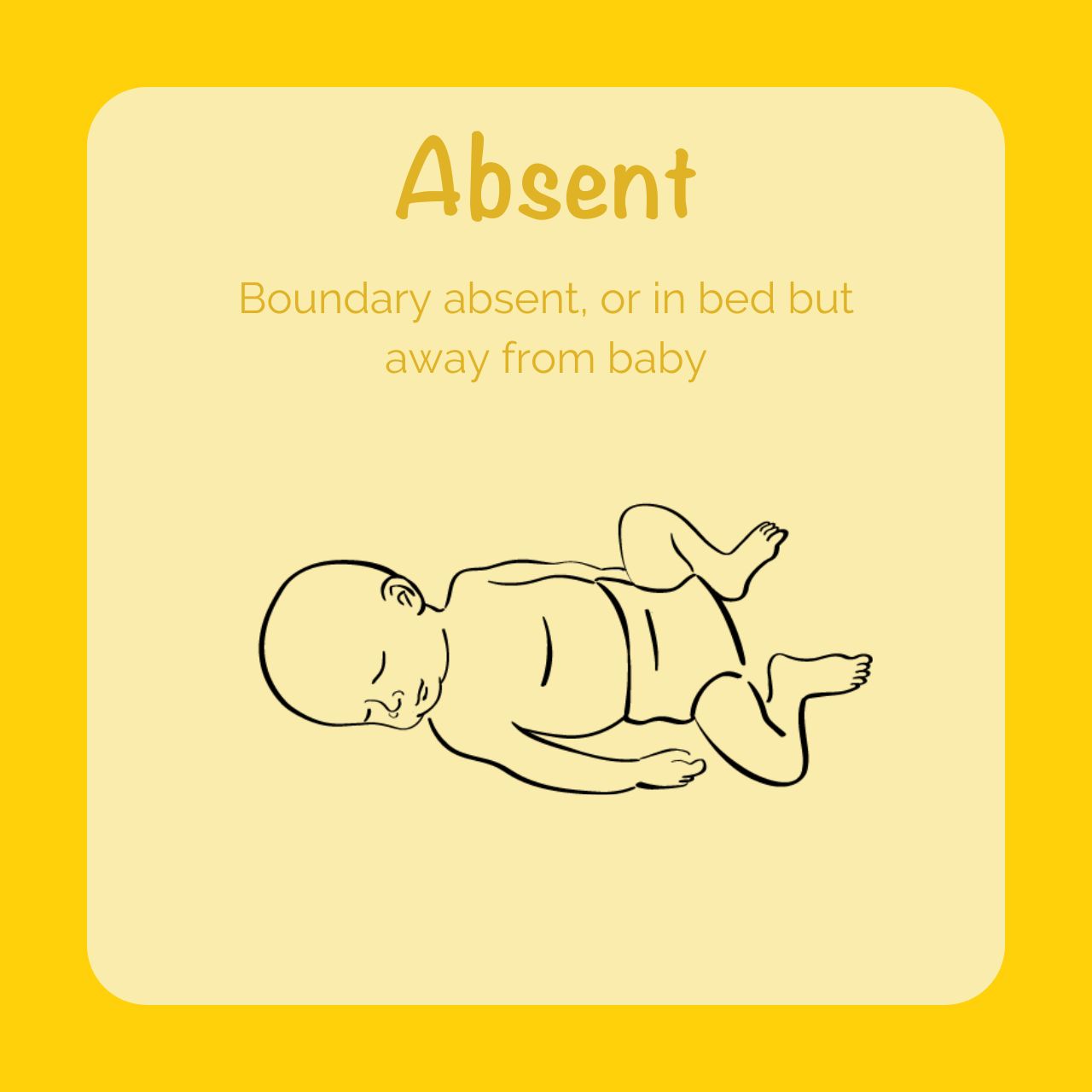
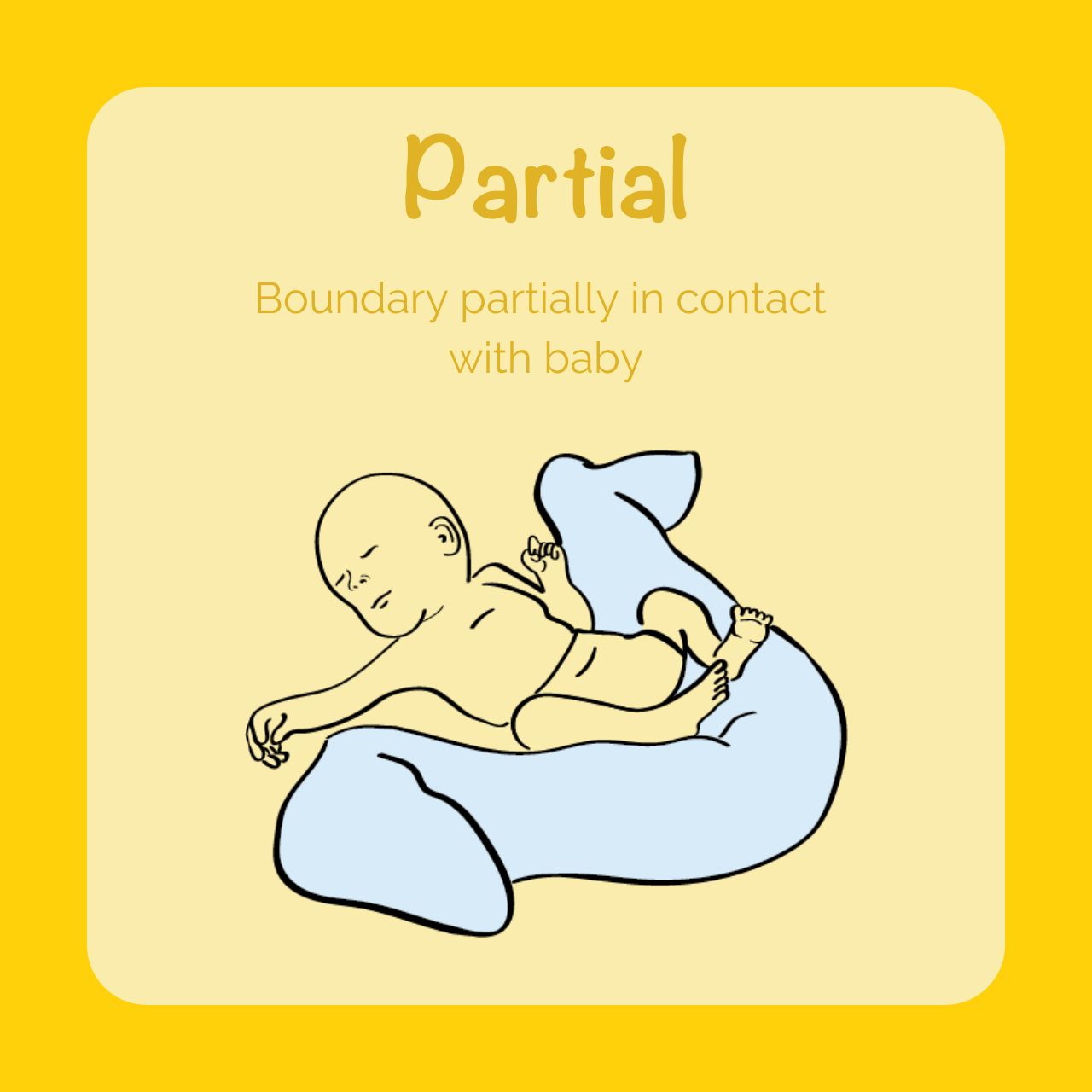
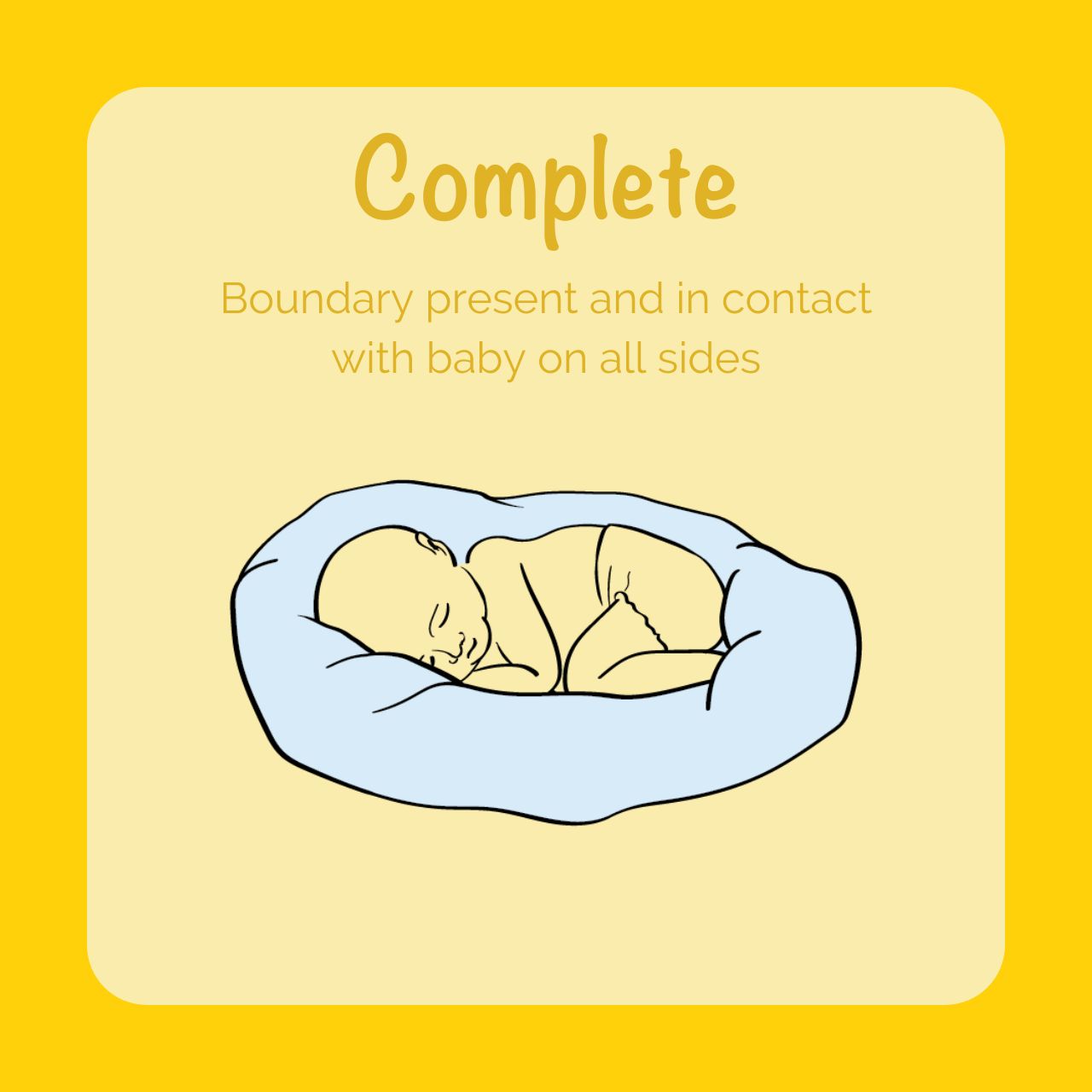
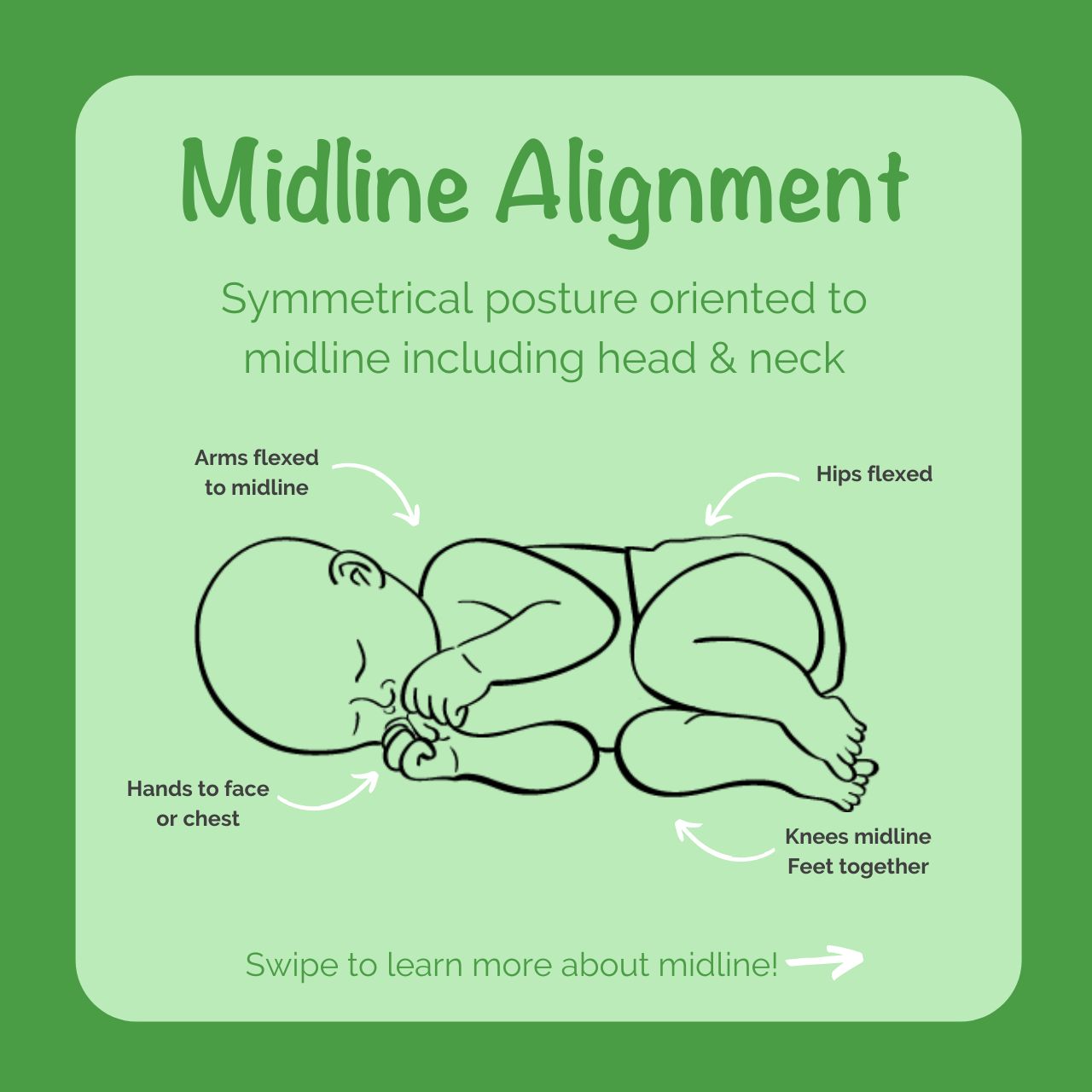
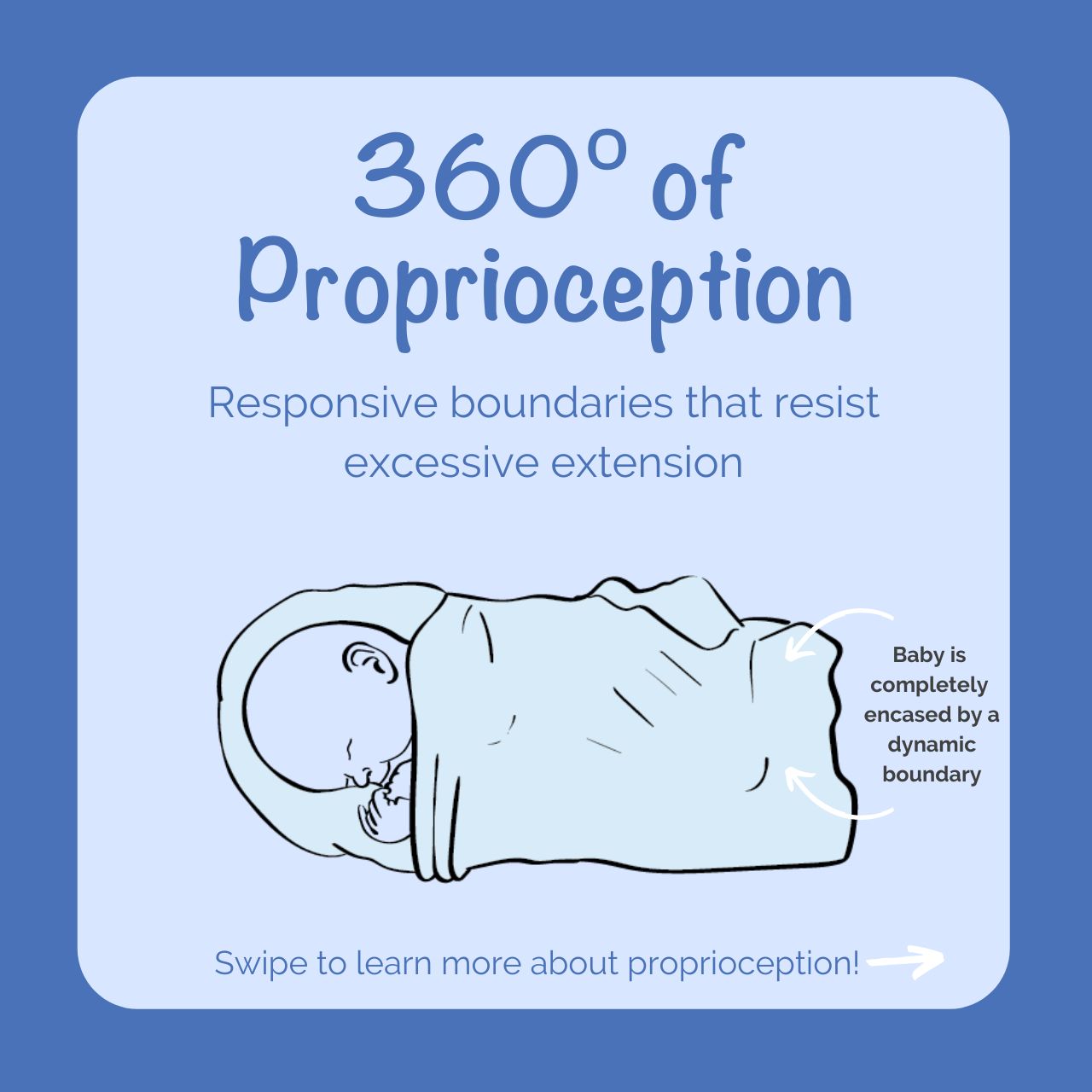
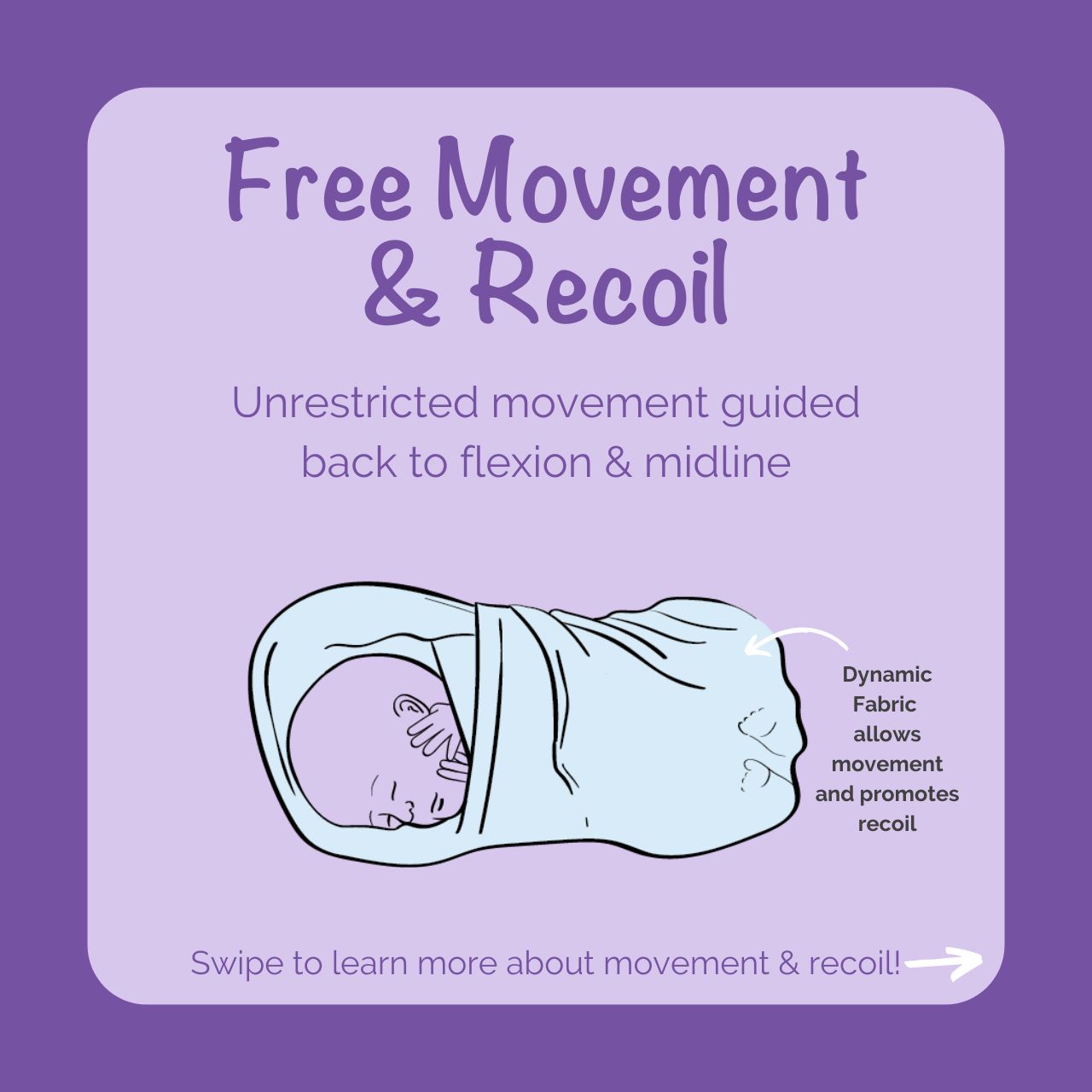
When determining “positional stability,” each infant’s medical and developmental needs should be considered before removing developmental positioning supports at a predetermined gestational age. Choosing a wearable blanket or swaddle that promotes flexion of the extremities provides dynamic support, allowing free movement while promoting passive recoil to a flexed posture is a reasonable option that supports positional stability and meets the AAP guideline for Safe Sleep. This dynamic relationship between baby and boundary is an essential component of healthy physical and sensory development.
Developmentally speaking, removing positioning aids early in the 3rd trimester may deprive the baby of the increasing physiologic flexion they would have experienced in the womb, which is vital to bone and muscle development.
- A 32-week infant, for example, should still experience an additional 6-8 weeks of pregnancy before neurologic and physical development are optimal. However, not every 32-week infant is the same physiologically or neurodevelopmentally.
- A 32-week baby born at 24 weeks gestation may have dramatically different physical and sensory support needs than a 32-week baby born at 31 weeks gestation.
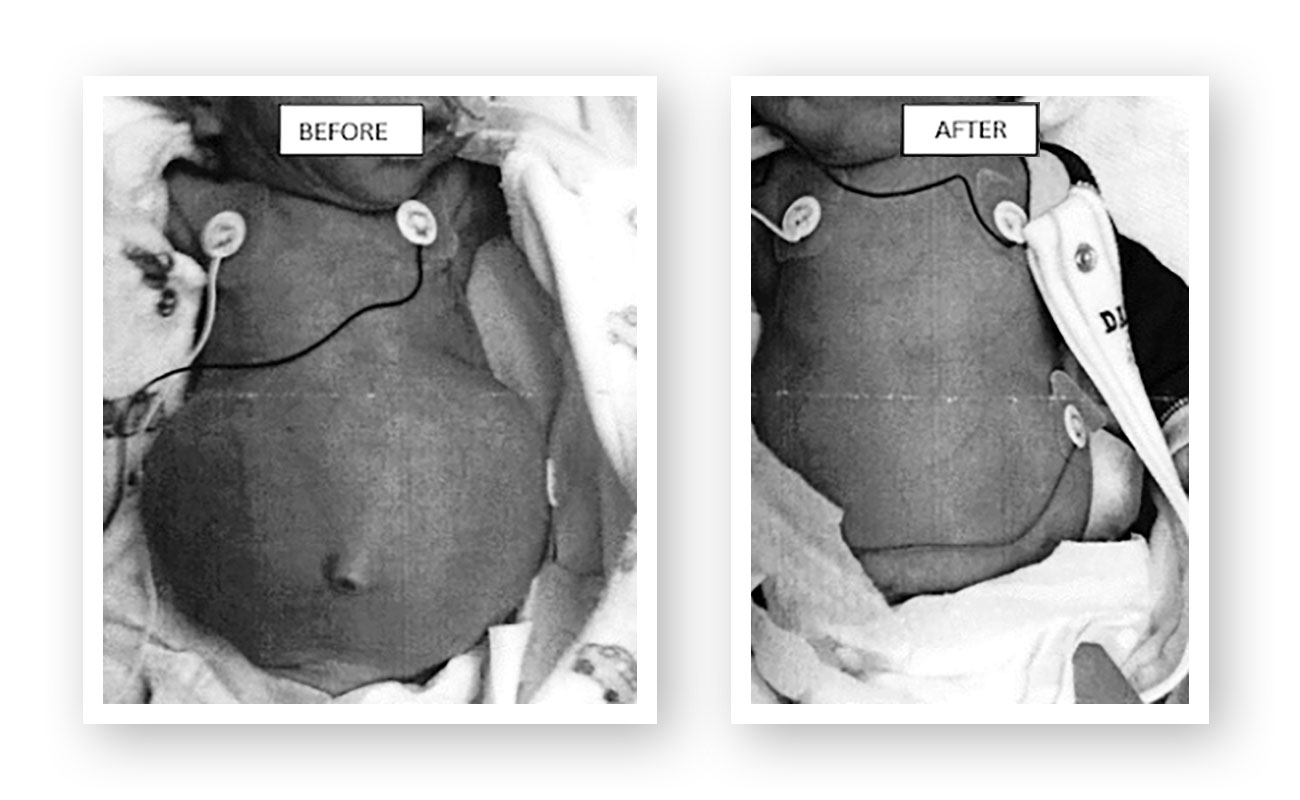
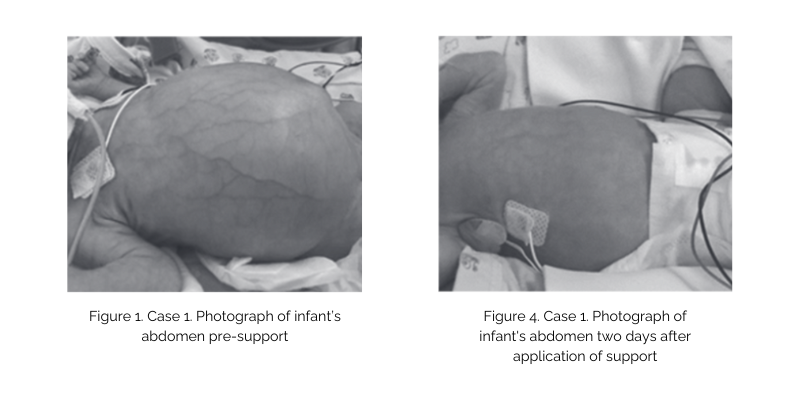
- Babies born at earlier gestational ages with more severe illnesses or congenital anomalies may require robust developmental support beyond reaching full term, making traditional swaddles and wearable blankets ineffective in meeting their needs.
Positioning with Purpose
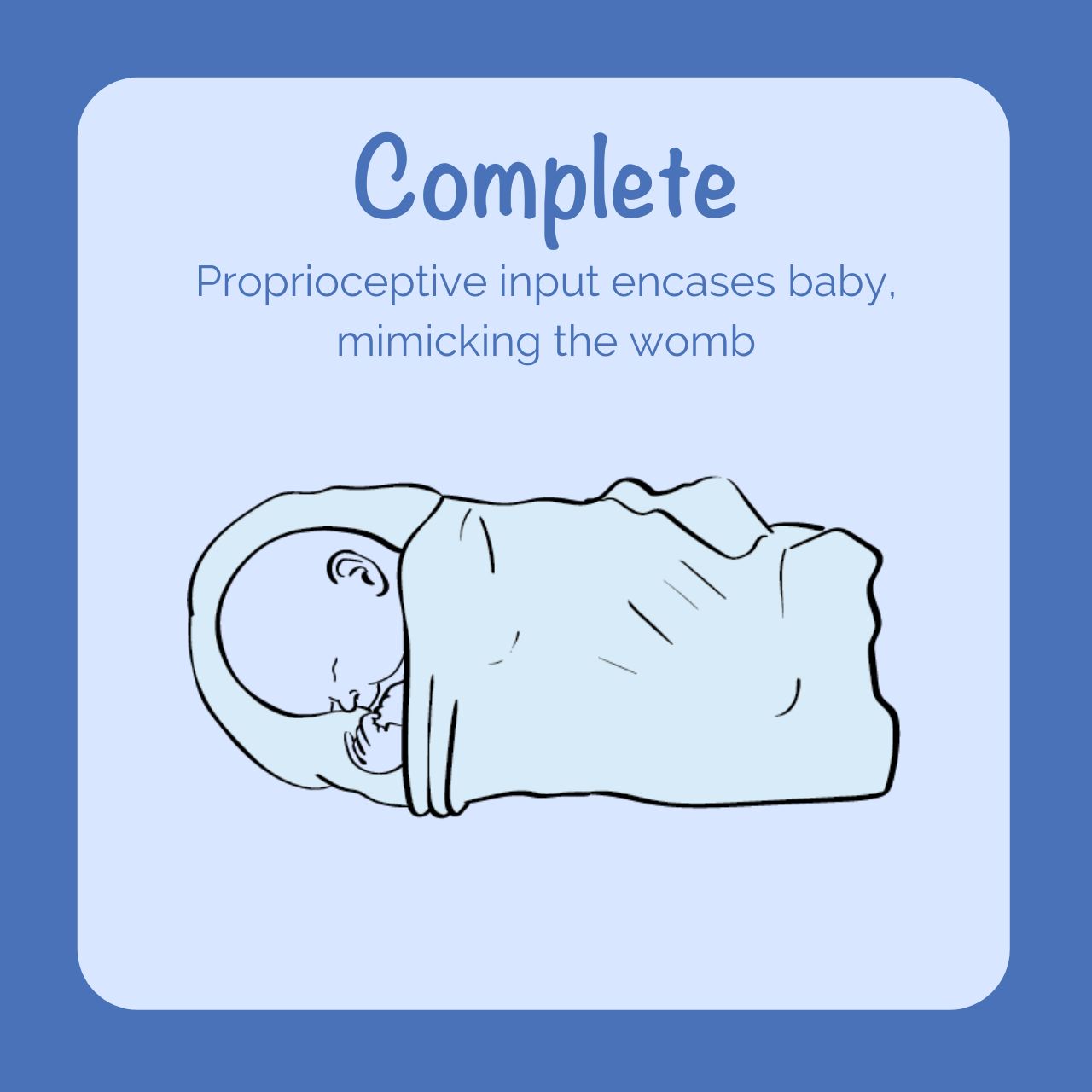
In the third trimester, the “resistance training” provided by the baby’s interaction with the dynamic, muscular boundary of the uterus facilitates proper development of the bones, muscles, and joints. Preterm infants are born prior to the completion of the third trimester, placing them at risk for altered physical development.
- Research evidence demonstrates that active resistive movement is essential for skeletal development along with maximized infant nutrition.
- The interaction between the baby and the muscular-responsive uterus is essential in loading bones sufficiently to maximize bone accretion.
- During this formative period in pregnancy, an exponential increase in bone growth occurs, resulting in 80% of fetal bone being produced (Drake, 2022).
• Bone loading to optimize bone accretion
• Muscle development
• Self-regulation and calming
The Dandle® WRAP Stretch provides dynamic resistance to extension movements of the extremities while promoting the return to a flexed resting posture, mimicking the action of the uterus:
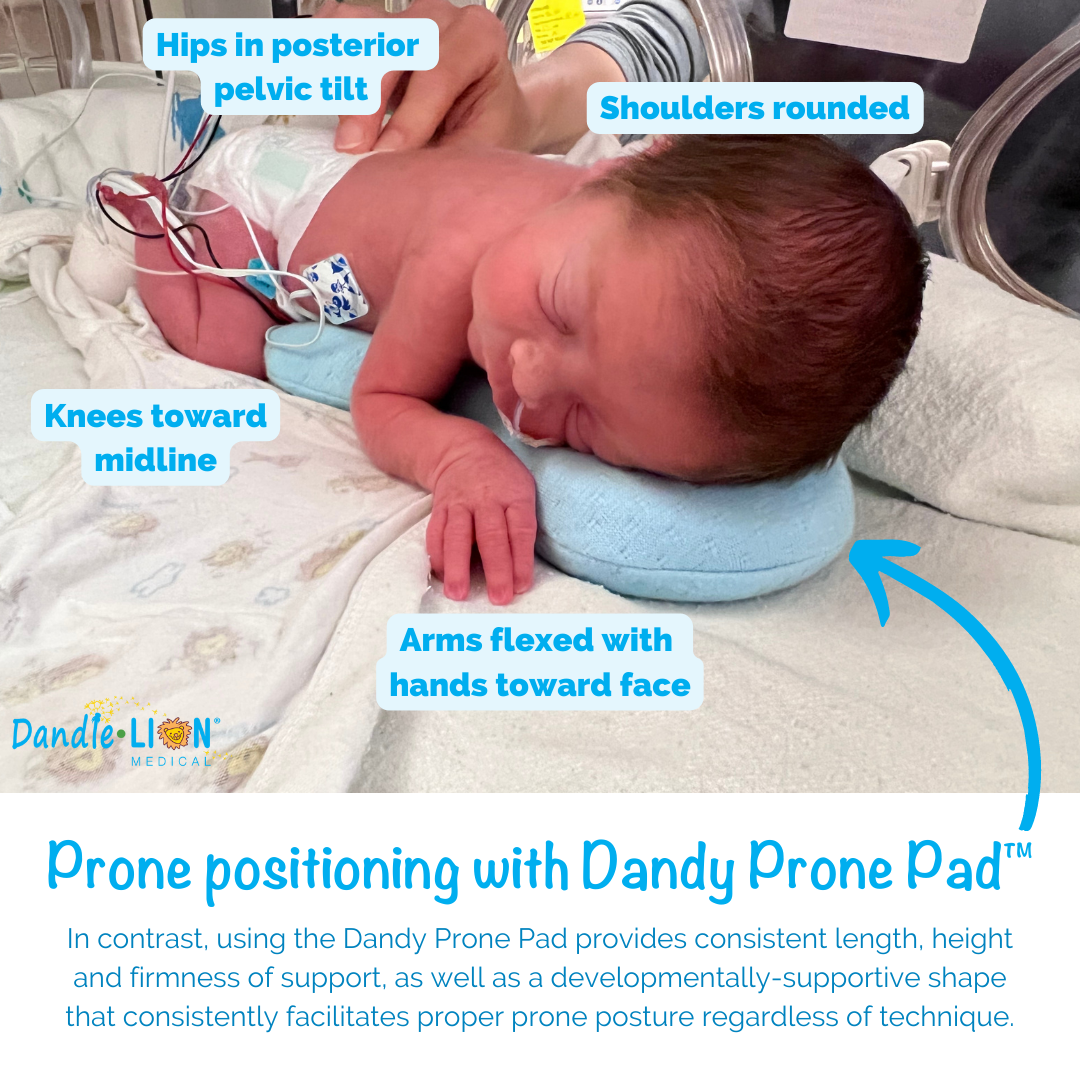
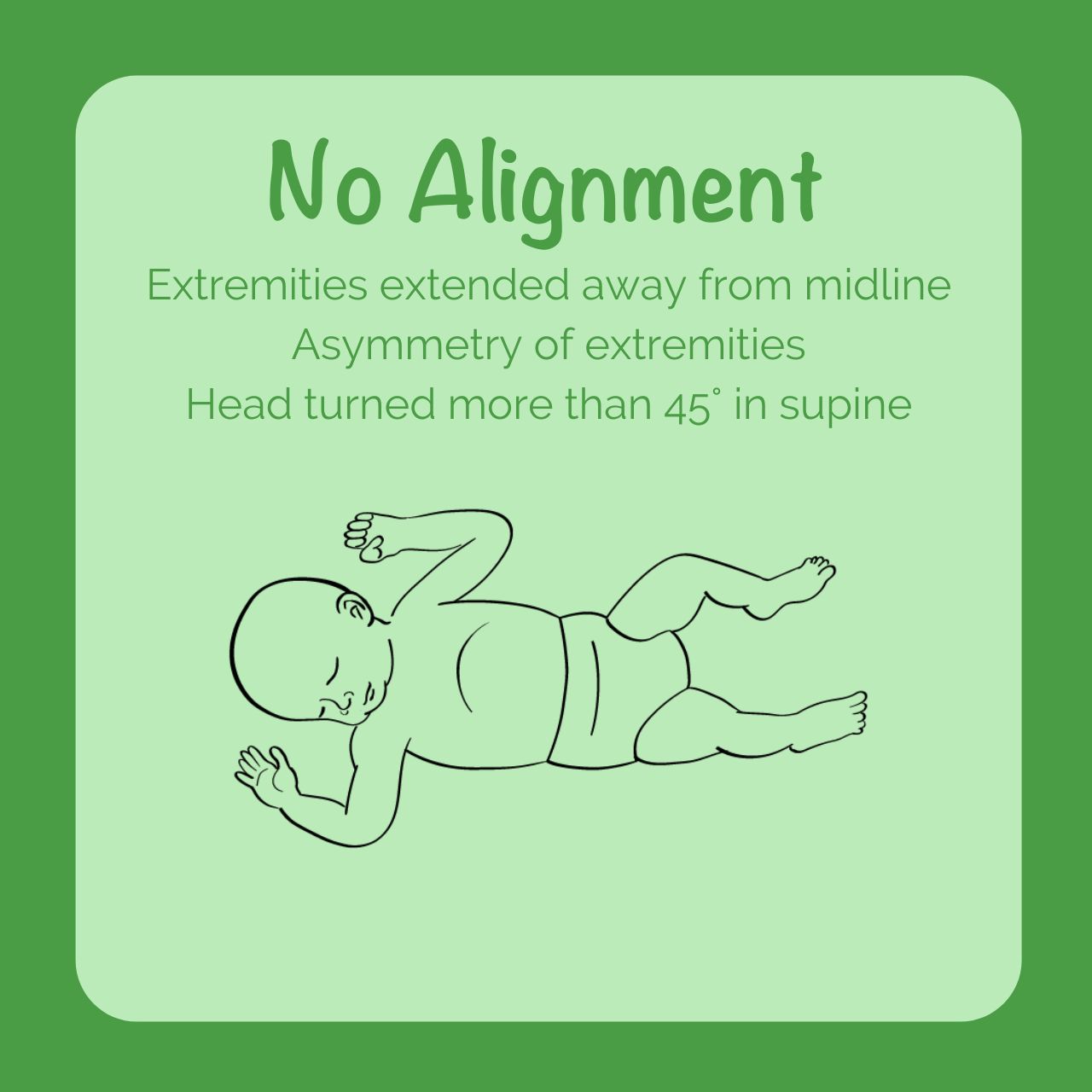
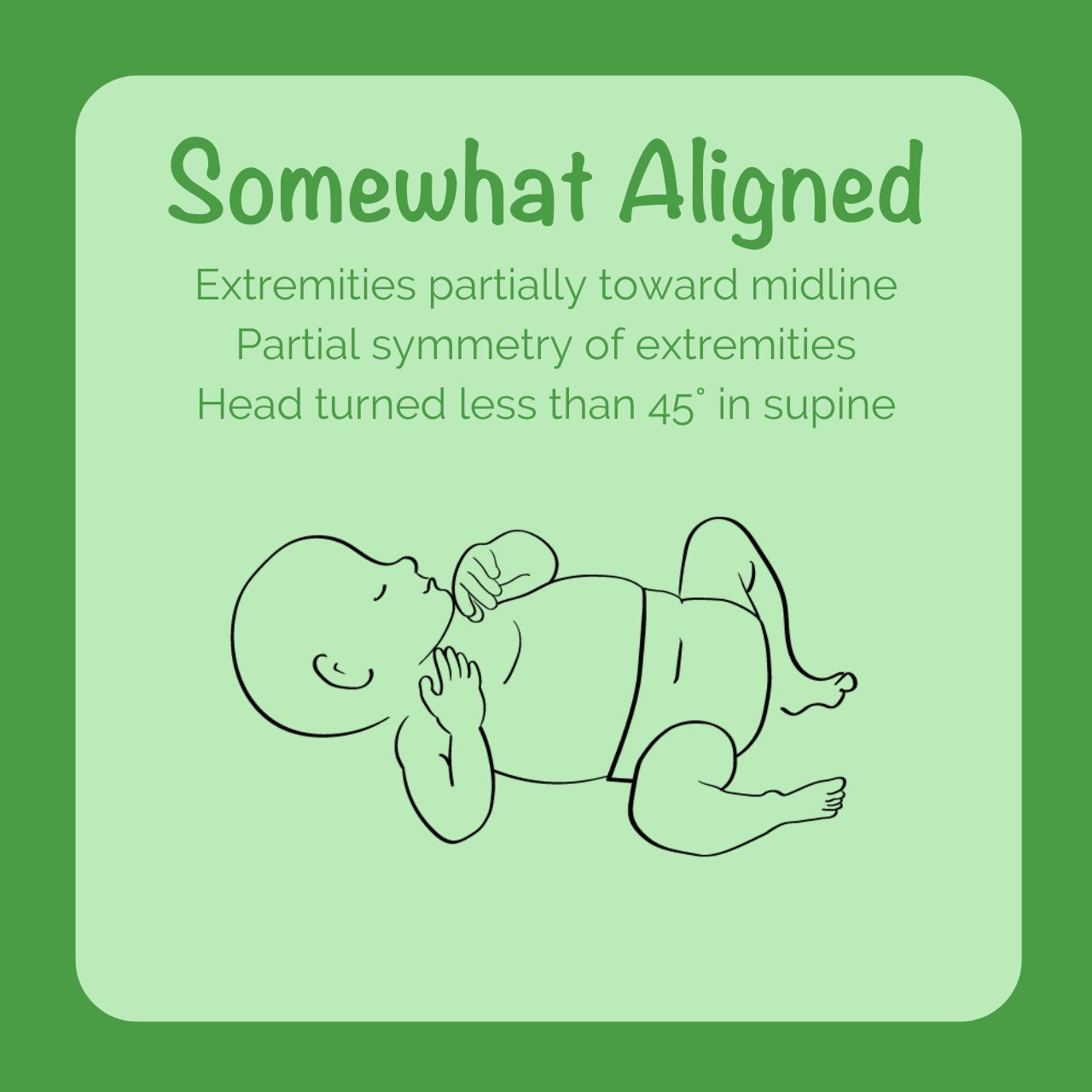
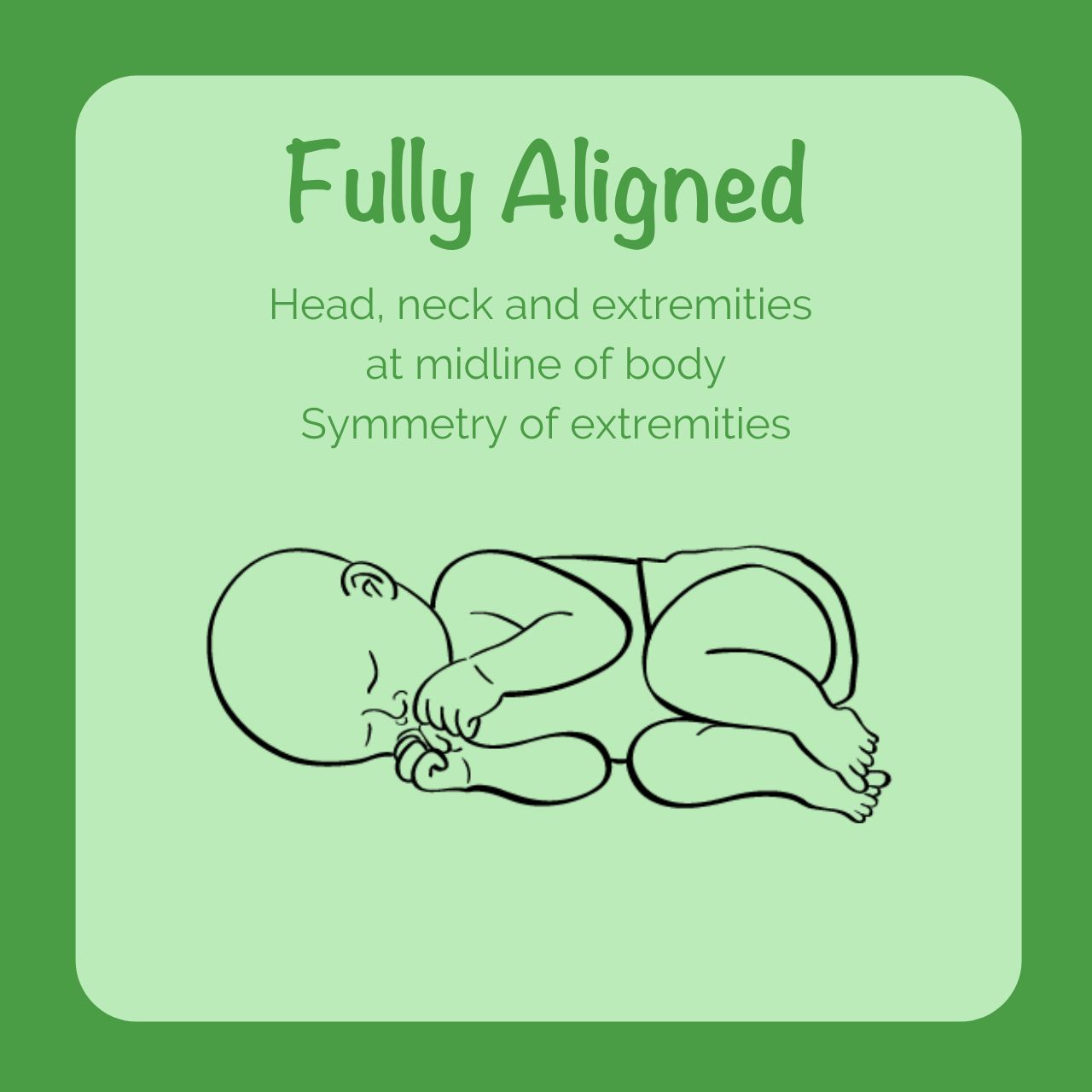
- Flexion and midline alignment of the infant in the womb is important for developing bones, joints, and muscles. This posture also facilitates self-regulation and calming, physiologic functions like digestion, and attainment of future motor milestones like rolling, crawling, and walking. Only when an infant can maintain this posture should they be considered as having obtained “positional stability.”
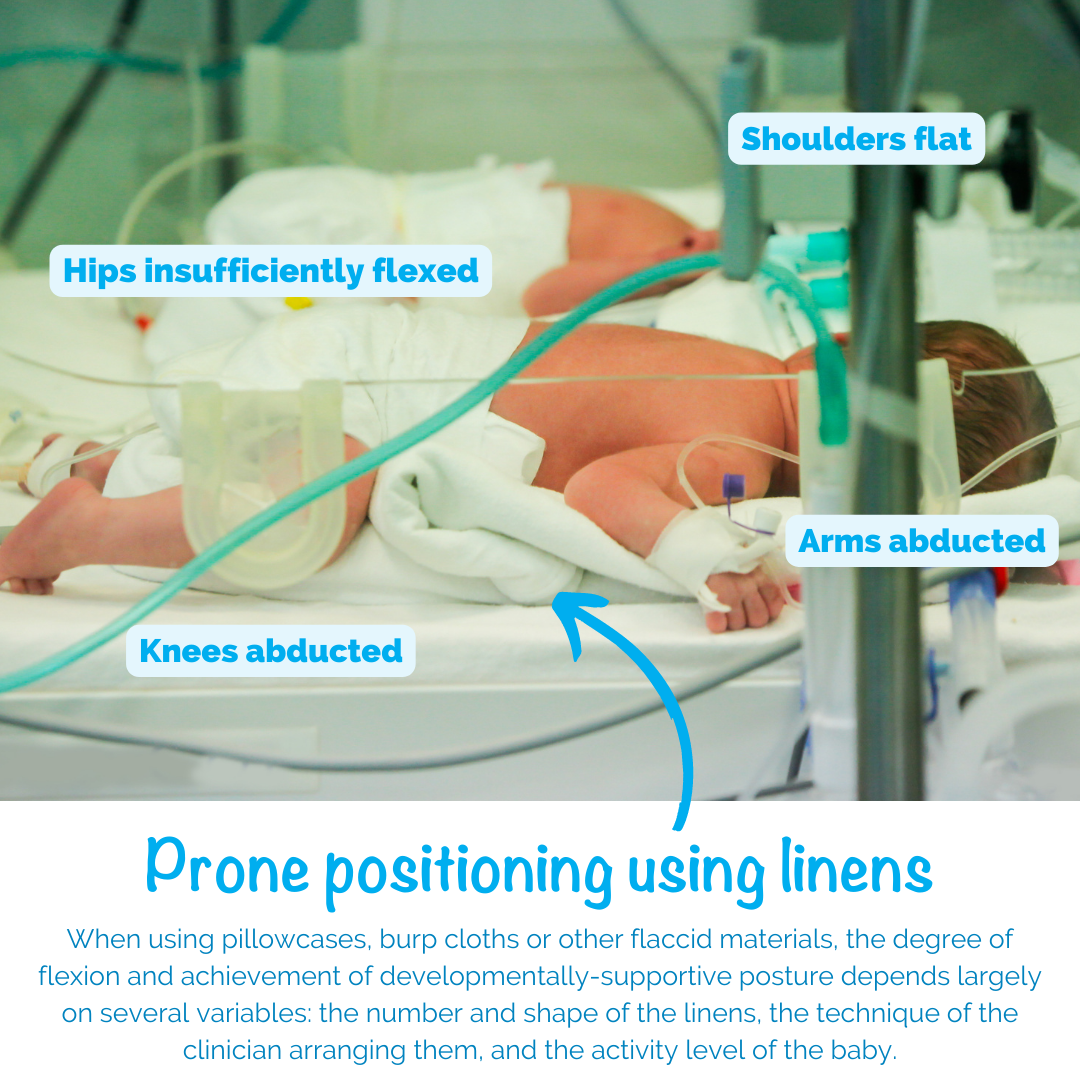
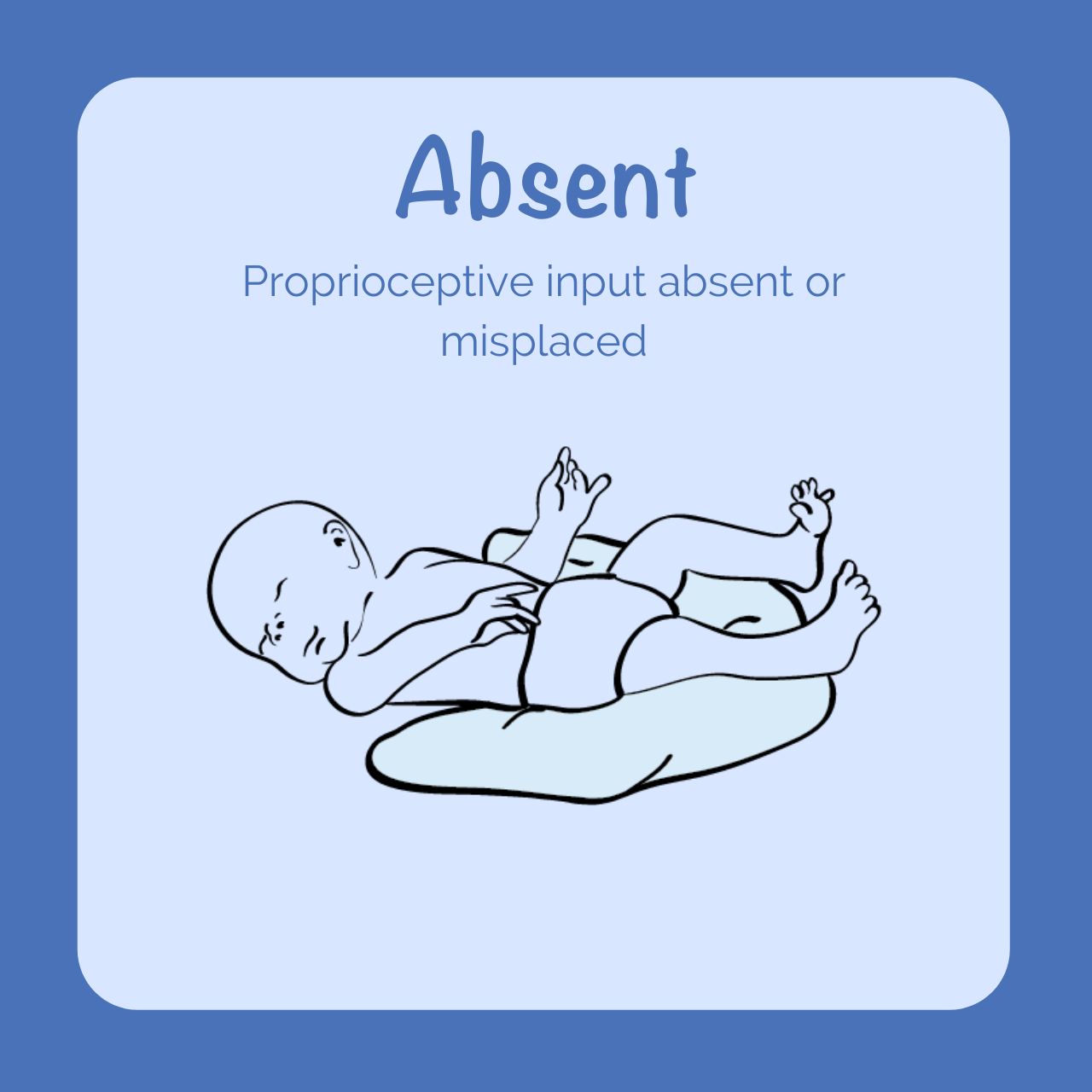
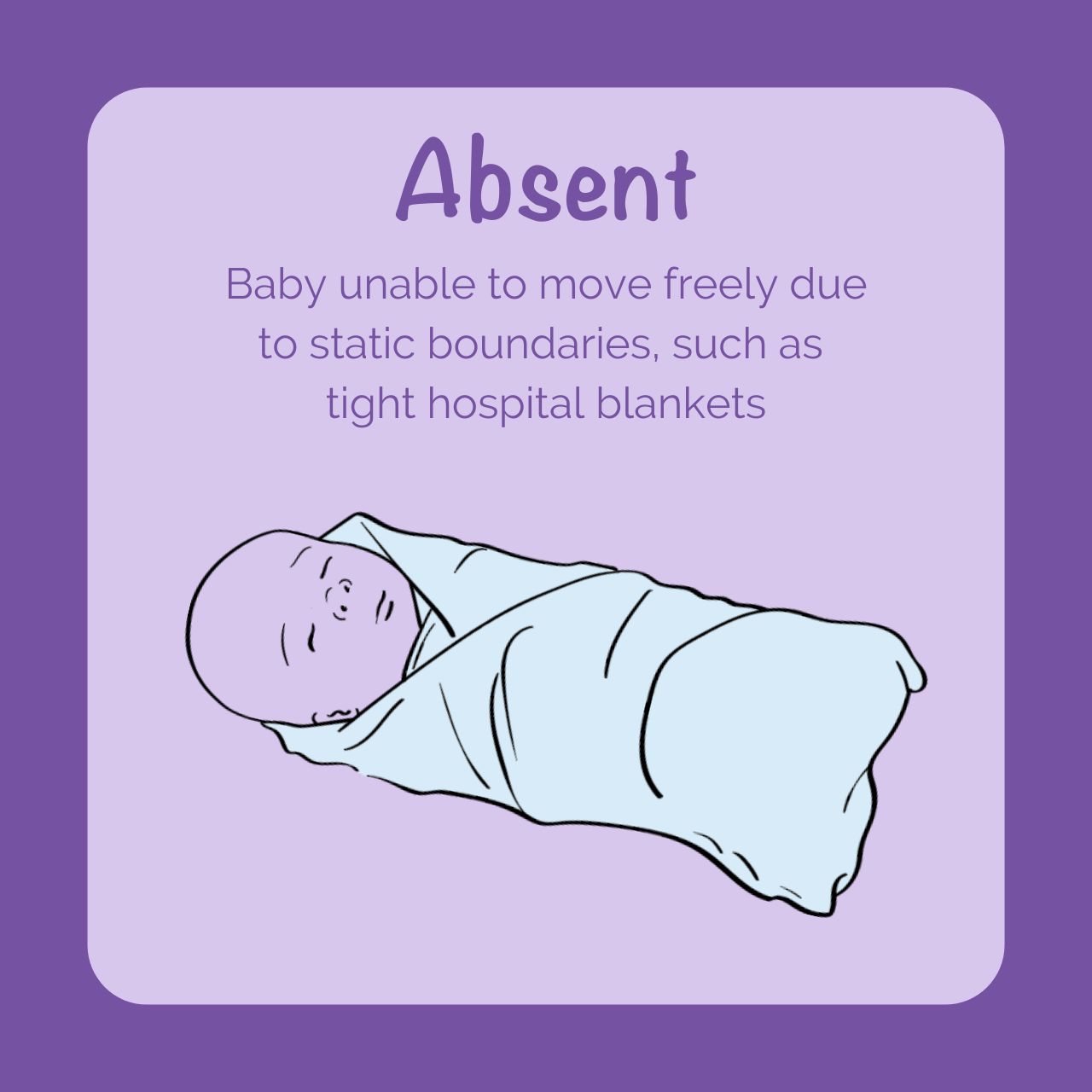
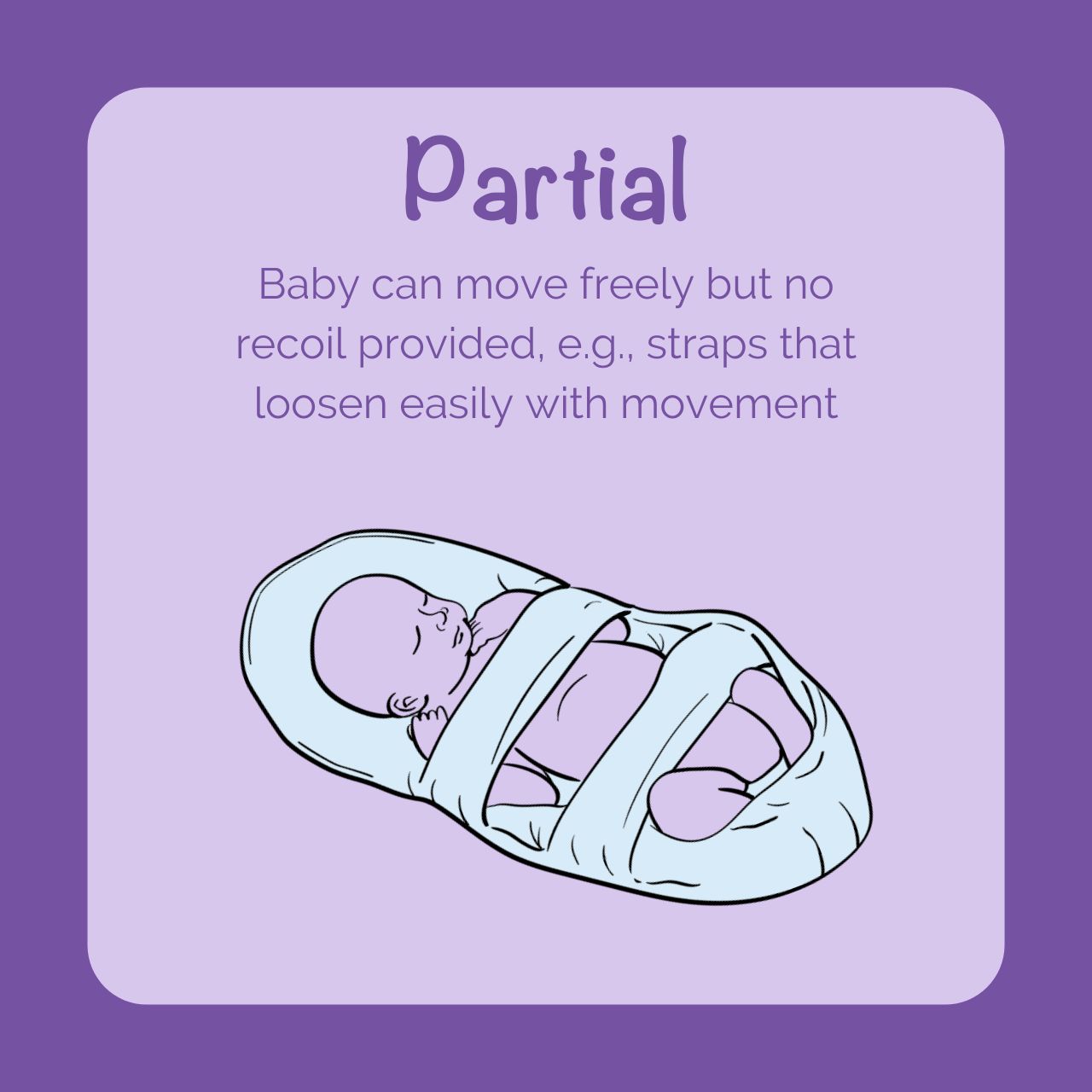
- Commercially available swaddles and sleep blankets generally allow for free movement, but when applied to preterm infants in the NICU, they often do not provide recoil or promote a consistently flexed, midline posture— leaving the lower extremities unsupported in extension.
As the Dandle WRAP Stretch is secured under the baby’s head and neck, it meets the definition of a wearable blanket/sleep sack, meeting both the safety and developmental needs of the infant. The physiologic importance of continued developmental support into the third trimester is clear. Providing babies with dynamic support by using a Dandle WRAP Stretch supports the infant’s musculoskeletal and sensory organizational needs while meeting the AAP 2022 recommendations.

Dandle•LION supports modeling Safe Sleep while encouraging hospitals to keep babies in their positioning aids for as long as possible within the context of their own unique policies/procedures around safe sleep. Our Dandle WRAP Stretch is compatible with AAP Safe Sleep recommendations and can be used even after “safe sleep” protocols have been implemented for a particular patient.
Learn more about the Dandle® WRAP Stretch here.
Sources:
Drake, L. (2022). Positioning the neonate for best outcomes. National Association of Neonatal Nurses.
Shea, C.; Rolfe, R.; and Murphy, P. The importance of foetal movement for coordinated cartilage and bone development in utero. Cone Joint Res, 2015: 7:105-116. Doi:10.1302/2046-3758.47.20000387.