Are you concerned about abdominal distension?
Continuous Positive Airway Pressure (CPAP) is a widely used respiratory support for preterm infants. However, concerns about abdominal distension due to CPAP, often referred to as “CPAP belly,” have sparked discussions about its potential sequelae and called for innovative solutions.
In this blog, Ginny McGill discusses her journey with CPAP Belly. Ginny is the author of “Neonatal abdominal support to address CPAP belly: Two case reports and literature review” and the creator of the NeoBellyBand.
A Simple Strategy for a Common Problem
As a physical therapist working in NICUs for over 20 years, I have seen the miraculous work done to save the lives of premature infants. Neonatal therapists often enter this environment with an eye toward addressing or preventing the consequences of prematurity. From positioning in flexion rather than flat on a bed to modifying the environment to meet the needs of immature senses, many simple ideas have improved the care of these infants.
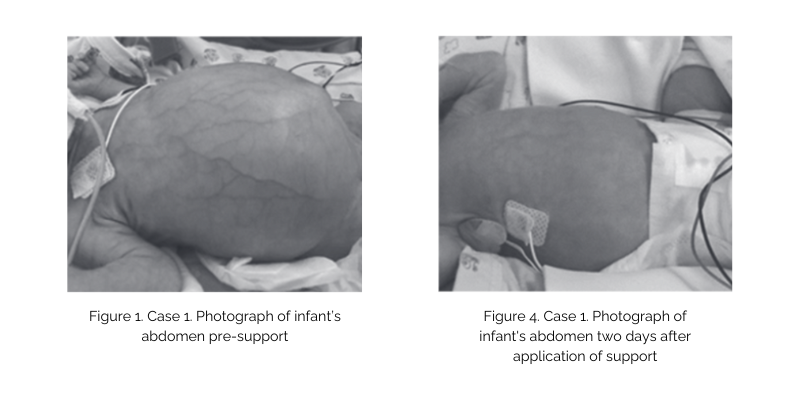
When observing bellies bloated by CPAP, I saw muscles that were stretched outside of their effective line of pull, placing the musculoskeletal system at a disadvantage to take over respiration after CPAP was removed. I saw arching and discomfort. This led me to embark on a journey to address and possibly prevent this unintended consequence of respiratory support.
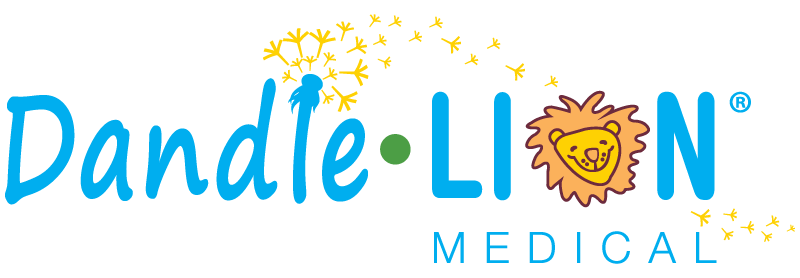
The first attempts were on older infants to rehabilitate their weak abdomens after CPAP had been discontinued. The first trial involving half-time wear of an abdominal support resulted in these changes:
This inspired further work, development of safety criteria, and trying on younger and younger babies to work towards prevention of CPAP belly. Prevention hoped to not just preserve muscle length and function but also to avoid the escalations in support sometimes used to try to overcome the respiratory inhibition which results from air in the GI system. I published two cases, one of treatment and one of prevention. When presenting these cases at a conference, it was clear this is a common issue from the line of therapists who stayed to discuss this further.
As one therapist in Anchorage, Alaska, with a simple idea, how do you help all these therapists? We are taught to communicate our work by publishing and presenting, and I had done that. And while I continue to gather data and prepare for further publication, it was obvious therapists were seeking support to help infants in their units. Some had already tried with different materials and differing success. I had done the groundwork, now how to get consistency in use for all these different units?
I am grateful Dandle•LION has been a partner in this cause. As a wise friend once said to me, you can do anything, but you can’t do everything. With a mind to provide consistency and safety for further use and study, the NeoBellyBand was born. Product development allows us all to know we are using what was used through the years of my CPAP belly journey and to know further study is all testing the same thing done the same way.
During this ongoing journey, the list of concerns about gaseous distension I hear from clinicians continues to expand. I started with weakness and concern for postural support for respiration now and movement development later. Those concerns expanded to the acute complications of distension during respiratory support, like the need for escalation of support to overcome a big belly. Others have expressed concerns about GI complications from feeding tolerance to SIP and still others the long-term consequences of visceral distension on digestion and possibly leading to ongoing inflammation.
These journeys take time, and all begin with one step. And while mine started on my own with a simple idea, it takes a team to make change. Thanks to Dandle•LION and all the clinicians I have spoken with since sharing this idea, who all hope to continue this journey towards improving the care of premature infants.
You are welcome to visit neophysicaltherapy.com to learn more and participate in the conversation, including what parents are saying.

by Ginny McGill, PT, DPT, CNT, NTMTC

Ginny McGill graduated from Creighton University with a Doctorate in Physical Therapy in 2001. She has practiced in the NICU for 22 years, at Phoenix Children’s Hospital and Providence Alaska Children’s Hospital. She has received certifications in Neonatal Therapy, Neonatal Touch and Massage, as well as wound care and lymphedema. Ginny teaches locally and nationally. You may have seen her speak through her work with the Vermont Oxford Network (VON), Engage Grow Thrive, or Creative Therapy Consultants.